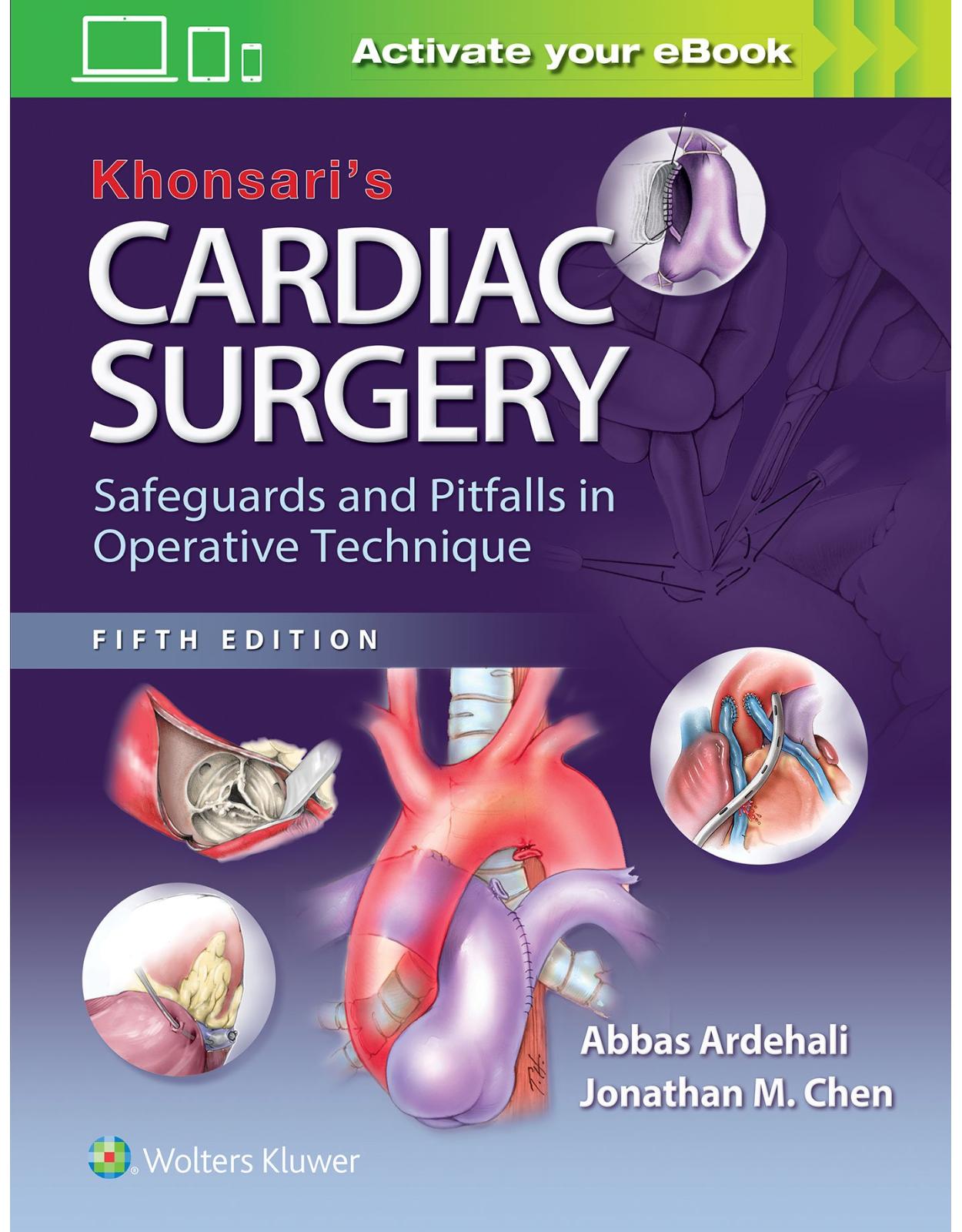
Khonsari’s Cardiac Surgery: Safeguards and Pitfalls in Operative Technique
Livrare gratis la comenzi peste 500 RON. Pentru celelalte comenzi livrarea este 20 RON.
Disponibilitate: La comanda in aproximativ 4 saptamani
Editura: LWW
Limba: Engleza
Nr. pagini: 448
Coperta: Hardcover
Dimensiuni: 21.84 x 2.03 x 27.94 cm
An aparitie: 05 Oct 2016
Description:
Unique in the field of cardiac surgery, Khonsari's Cardiac Surgery: Safeguards and Pitfalls in Operative Technique details the most important techniques in a concise, readable, and richly illustrated format, with a focus on avoiding and managing surgical pitfalls and complications. From general considerations through the surgical correction of acquired and congenital heart conditions, it provides a wealth of practical, hands-on guidance to help both seasoned and less-experienced cardiac surgeons achieve optimal outcomes. Key Features: •Apply the very latest know-how with new sections on endovascular procedures, transcatheter aortic valve replacement (TAVR), new approaches to Norwood reconstruction and repair of Ebstein anomaly, and alternative anatomic repairs of congenitally corrected transposition, as well as thorough updates to all chapters.•Master nuances of surgical technique thanks to a wealth of step-by-step illustrations, many of them new, others colorized for greater clarity.•Optimize outcomes with special coverage of avoiding and managing technical pitfalls and complications.•Spot important details with the aid of distinctive "Nota Bene" notations.Now with the print edition, enjoy the bundled interactive eBook edition, offering tablet, smartphone, or online access to: •Complete content with enhanced navigation•A powerful search that pulls results from content in the book, your notes, and even the web•Cross-linked pages, references, and more for easy navigation•Highlighting tool for easier reference of key content throughout the text•Ability to take and share notes with friends and colleagues•Quick reference tabbing to save your favorite content for future use
Table of Contents:
Section I: General Considerations
Chapter 1: Surgical Approaches to the Heart and Great Vessels
Primary Median Sternotomy
Technique
Figure 1.1
Figure 1.2
Figure 1.3
Repeat Sternotomy
Technique
Figure 1.4
Figure 1.5
Figure 1.6
Figure 1.7
Figure 1.8
Sternal Closure
Technique
Figure 1.9
Figure 1.10
Figure 1.11
Figure 1.12
Postoperative Sternal Wound Infection
General Considerations
Specific Technical Considerations
Pectoralis Muscle Flap
Technique
Superior Rectus Flap
Technique
Myocutaneous Flap
Technique
Figure 1.13
Thoracotomy
Alternative Surgical Approaches
Full Sternotomy through Submammary Incision
Technique
Full Sternotomy through a Limited Midline Incision
Technique
Lower Ministernotomy
Technique
Lower Ministernotomy Closure
Upper Ministernotomy
Technique
Submammary Right Thoracotomy
Technique
Closure of Submammary Right Thoracotomy
Figure 1.14
Figure 1.15
Figure 1.16
Figure 1.17
Figure 1.18
Figure 1.19
Figure 1.20
Chapter 2: Preparation for Cardiopulmonary Bypass
Exposure of the Heart
Technique
Dissection Around the Aorta
Dissection Around the Cavae
Figure 2.1
Figure 2.2
Figure 2.3
Figure 2.4
Figure 2.5
Figure 2.6
Figure 2.7
Figure 2.8
Arterial Cannulation
Aortic Cannulation
Technique
Femoral Artery Cannulation
Technique
Axillary Artery Cannulation
Technique
Transapical Aortic Cannulation
Technique
Figure 2.9
Figure 2.10
Figure 2.11
Figure 2.12
Figure 2.13
Figure 2.14
Figure 2.15
Figure 2.16
Venous Cannulation
Right Atrial Cannulation
Technique
Bicaval Cannulation
Technique
Technique of Direct Caval Cannulation
Inferior Vena Cava
Superior Vena Cava
Femoral Venous Cannulation
Technique
Adequacy of Bypass
Signs of Aortic Dissection
Improper Positioning of Caval Cannula
Retrograde Aortic Dissection
Traumatic Disruption and Dissection of the Ascending Aorta
Figure 2.17
Figure 2.18
Figure 2.19
Figure 2.20
Figure 2.21
Figure 2.22
Figure 2.23
Figure 2.24
Figure 2.25
Chapter 3: Myocardial Preservation
Chapter 3 Introduction
Aortic Root Infusion Technique
Direct Coronary Artery Perfusion
Figure 3.1
Myocardial Preservation by the Retrograde Perfusion Method
Technique
Retrograde Cardioplegic Infusion by the Open Technique
Figure 3.2
Figure 3.3
Chapter 4: Venting and Deairing of the Heart
Chapter 4 Introduction
Left Ventricular Apical Venting
Technique
Figure 4.1
Figure 4.2
Venting through the Right Superior Pulmonary Vein
Figure 4.3
Figure 4.4
Venting through the Superior Aspect of the Left Atrium
Figure 4.5
Pulmonary Artery Venting
Figure 4.6
Venting through the Foramen Ovale
Technique
Deairing of the Heart
Section Ii: Surgery for Acquired Heart Disease
Chapter 5: Surgery of the Aortic Valve
Chapter 5 Introduction
Surgical Anatomy of the Aortic Valve
Figure 5.1
Approach to the Aortic Valve
Myocardial Preservation
Technique
Exposure of the Aortic Valve by Transverse Aortotomy
Exposure of the Aortic Valve by Oblique Aortotomy
Figure 5.2
Figure 5.3
Figure 5.4
Aortic Valve Replacement
Excision of the Aortic Valve
Sizing the Aortic Prosthesis
Technique for Suture Insertion
Seating the Prosthesis
Aortotomy Closure
Technique
Figure 5.5
Figure 5.6
Figure 5.7
Figure 5.8
Figure 5.9
Figure 5.10
Figure 5.11
Figure 5.12
Figure 5.13
Figure 5.14
Figure 5.15
Figure 5.16
Figure 5.17
Figure 5.18
Figure 5.19
Figure 5.20
Figure 5.21
Figure 5.22
Figure 5.23
Figure 5.24
Figure 5.25
Figure 5.26
Figure 5.27
Figure 5.28
Homograft, Autograft, and Porcine Stentless Aortic Root in Aortic Valve Replacement
Technique: Pulmonary Autograft Replacement of the Aortic Root: the Ross Procedure
Technique: Aortic Valve Replacement Using Stentless Bioprosthesis or Aortic Homograft
Figure 5.29
Figure 5.30
Figure 5.31
Figure 5.32
Figure 5.33
Figure 5.34
Figure 5.35
Figure 5.36
Figure 5.37
Figure 5.38
Figure 5.39
Figure 5.40
Figure 5.41
Figure 5.42
Figure 5.43
Figure 5.44
Figure 5.45
Figure 5.46
Figure 5.47
Figure 5.49
Figure 5.48
Figure 5.50
Figure 5.51
Figure 5.52
Figure 5.53
Figure 5.54
Aortic Valve Repair
Techniques
Figure 5.55
Figure 5.56
Figure 5.57
Problematic Cases
Management of Unclampable Aorta
Technique
Apicoaortic Valve Conduit
Technique
Management of the Small Aortic Root
Tilted Prosthesis Technique
Patch Enlargement Technique
Endocarditis
Figure 5.58
Figure 5.59
Figure 5.60
Figure 5.61
Figure 5.62
Figure 5.63
Paravalvular Leaks
Technique for Repair
Figure 5.64
Transcatheter Aortic Valve Replacement
Patient Selection
Operative Technique
Figure 5.65
Figure 5.66
Chapter 6: Surgery of the Mitral Valve
Chapter 6 Introduction
Surgical Anatomy of the Mitral Valve
Technical Considerations
Incision
Myocardial Preservation
Exposure of the Mitral Valve
Interatrial Groove Approach
Transatrial Oblique Approach
Transatrial Longitudinal Septal Approach
Figure 6.1
Figure 6.2
Figure 6.3
Figure 6.4
Figure 6.5
Figure 6.6
Figure 6.7
Figure 6.8
Figure 6.9
Open Mitral Commissurotomy for Mitral Stenosis
Figure 6.10
Closed Mitral Commissurotomy for Mitral Stenosis
Technique
Conversion of a Closed Mitral Valvotomy to the Open Technique
Figure 6.11
Figure 6.12
Figure 6.13
Mitral Valve Reconstruction
Reconstruction of the Mitral Valve Leaflets
Quadrangular or Triangular Resection
Creation of Artificial Chordae
Gore-Tex Chordal Replacement
Technique
Edge-to-Edge Mitral Valve Repair
Technique
Anterior Mitral Leaflet Abnormalities
Technique
Reconstruction of the Mitral Valve Annulus
Commissuroplasty
Annuloplasty
Complete Mitral Annuloplasty Ring
Technique
Incomplete Mitral Annuloplasty Ring
Technique
Reconstruction of the Chordae Tendineae
Attachment of the Chords to the Mitral Leaflets
Ischemic Mitral Regurgitation
Figure 6.14
Figure 6.15
Figure 6.16
Figure 6.17
Figure 6.18
Figure 6.19
Figure 6.20
Figure 6.21
Figure 6.22
Figure 6.23
Figure 6.24
Figure 6.25
Mitral Valve Replacement
Technique
Technique for Chord Replacement
Sizing the Mitral Orifice
Valve Choices
Technique for Suture Insertion
Mitral Valve Replacement in Children
Figure 6.26
Figure 6.27
Figure 6.28
Figure 6.29
Figure 6.30
Figure 6.31
Figure 6.32
Figure 6.33
Figure 6.34
Figure 6.35
Figure 6.36
Figure 6.37
Figure 6.38
Figure 6.39
Figure 6.40
Figure 6.41
Late Annular Complications
Posterior Subannular Aneurysm
Paravalvular Leaks
Figure 6.42
Atrial Closure
Interatrial Groove Approach
Transatrial Oblique Approach
Transatrial Longitudinal Septal Approach
Figure 6.43
Figure 6.44
Figure 6.45
Chapter 7: Surgery of the Tricuspid Valve
Chapter 7 Introduction
Technical Considerations
Surgical Anatomy of the Tricuspid Valve and the Right Ventricle
Incision
Cannulation
Exposure of the Tricuspid Valve
Figure 7.1
Figure 7.2
Figure 7.3
Functional Tricuspid Regurgitation
Technique
De Vega Annuloplasty
Ring Annuloplasty
Bicuspidization of the Tricuspid Valve
Figure 7.4
Figure 7.5
Figure 7.6
Figure 7.7
Organic Tricuspid Valve Disease
Rheumatic Tricuspid Disease
Technique of Tricuspid Commissurotomy
Degenerative Tricuspid Disease
Technique
Pacemaker Lead–Induced Tricuspid Regurgitation
Figure 7.8
Tricuspid Valve Replacement
Tricuspid Valve Endocarditis
Figure 7.9
Figure 7.10
Figure 7.11
Figure 7.12
Chapter 8: Surgery of the Aorta
Acute Aortic Dissection
Figure 8.1
Aortic Aneurysms
Replacement of the Ascending Aorta
Retrograde Cerebral Perfusion
Selective Antegrade Cerebral Perfusion
Technique
Clamping of the Aorta
Myocardial Protection
Figure 8.2
Figure 8.3
Figure 8.4
Figure 8.5
Figure 8.6
Figure 8.7
Figure 8.8
Figure 8.9
Aortic Root Replacement
The Interposition Technique
Techniques for Aortic Root Replacement with a Bioprosthesis
Aortic Valve-Sparing Root Replacement
Figure 8.10
Figure 8.11
Figure 8.12
Figure 8.13
Figure 8.14
Figure 8.15
Figure 8.16
Figure 8.17
Technique for Replacement of an Aortic Arch Aneurysm
Elephant-Trunk Technique
Figure 8.18
Figure 8.19
Figure 8.20
Figure 8.21
Figure 8.22
Figure 8.23
Figure 8.24
Management of Type B Aortic Dissection
Technique for Replacement of the Descending Thoracic Aorta
Technique
Drainage of Cerebrospinal Fluid
Figure 8.25
Figure 8.26
Figure 8.27
Figure 8.28
Endovascular Repair of Descending Thoracic Aortic Aneurysms
Technique
Figure 8.29
Figure 8.30
Figure 8.31
Figure 8.32
Endovascular Repair of Aortic Arch Aneurysm
Technique
Figure 8.33
Figure 8.34
Chapter 9: Surgery for Coronary Disease
Chapter 9 Introduction
Technique for Internal Thoracic Artery Harvest
Figure 9.1
Technique for Radial Artery Harvest
Endoscopic Radial Artery Harvest
Open Radial Artery Harvest
Figure 9.2
Figure 9.3
Techniques for Greater Saphenous Vein Harvest
Endoscopic Saphenous Vein Harvest
Open Greater Saphenous Vein Harvest
Skin Closure
Figure 9.4
Figure 9.5
Figure 9.6
Figure 9.7
Figure 9.8
Figure 9.9
Figure 9.10
Figure 9.11
Figure 9.12
Figure 9.13
Coronary Artery Bypass Grafting with Cardiopulmonary Bypass
Myocardial Preservation
General Principles of Arteriotomy
Positioning the Heart to Expose Coronary Arteries
Exposure of the Anterior Surface of the Heart
Exposure of the Right Coronary Artery and Branches
Exposure of the Circumflex Coronary Artery and Branches
Anastomotic Techniques
Alternate Distal Anastomotic Techniques
Interrupted Suture Technique
Sequential Anastomosis
Toe-First Anastomosis
Endarterectomy
Technique
Proximal Anastomoses
Technique for Proximal Anastomosis
Figure 9.14
Figure 9.15
Figure 9.16
Figure 9.17
Figure 9.18
Figure 9.19
Figure 9.20
Figure 9.21
Figure 9.22
Figure 9.23
Figure 9.24
Figure 9.25
Figure 9.26
Figure 9.27
Figure 9.28
Figure 9.29
Figure 9.30
Figure 9.31
Figure 9.32
Figure 9.33
Figure 9.34
Figure 9.35
Figure 9.36
Figure 9.37
Figure 9.38
Figure 9.39
Figure 9.40
Figure 9.41
Figure 9.42
Figure 9.43
Figure 9.44
Figure 9.45
Figure 9.46
Figure 9.47
Figure 9.48
Figure 9.49
Figure 9.50
Figure 9.51
Figure 9.53
Figure 9.52
Figure 9.54
Figure 9.55
Figure 9.56
Figure 9.57
Figure 9.58
Figure 9.59
Figure 9.60
Figure 9.61
Figure 9.62
Figure 9.63
Figure 9.64
Figure 9.65
Figure 9.66
Figure 9.67
Off-Pump Coronary Artery Bypass Grafting
Anesthetic Considerations
Anterior Vessels
Left Anterior Descending and Diagonal Branch
Ramus Intermedius and High Obtuse Marginal Branches
Posterior Vessels: Obtuse Marginal Branches
Posterior Vessels
Posterior Descending Artery
Distal Right Coronary Artery
Conduct of the Surgery
Transmyocardial Revascularization
Technique
Figure 9.68
Figure 9.69
Figure 9.70
Figure 9.71
Figure 9.72
Figure 9.73
Figure 9.74
Figure 9.75
Figure 9.76
Figure 9.77
Figure 9.78
Figure 9.79
Figure 9.80
Considerations in Reoperative Coronary Artery Bypass Surgery
Chapter 10: Surgery for Mechanical Complications of Myocardial Infarction
Chapter 10 Introduction
Exposure and Cannulation of the Heart
Acute Myocardial Rupture
Ventricular Septal Rupture
Technique for the Surgical Treatment of a Ventricular Septal Defect
Figure 10.1
Figure 10.2
Figure 10.3
Figure 10.4
Papillary Muscle Rupture
Figure 10.5
Surgical Ventricular Restoration
Technique
Figure 10.6
Figure 10.7
Figure 10.8
Figure 10.9
Figure 10.10
Pseudoaneurysm
Ischemic Mitral Regurgitation
Intraaortic Balloon Pump
Technique for Placement of Intraaortic Balloon Pump
Figure 10.11
Chapter 11: Heart Transplantation
Chapter 11 Introduction
Donor Selection
Preservation Solution
Donor Operation
Figure 11.1
Figure 11.2
Figure 11.3
Recipient Surgery
Bicaval Technique
Figure 11.4
Figure 11.5
Figure 11.6
Figure 11.7
Chapter 12: Cardiac Tumors
Benign Tumors
Myxoma
Technique
Right Atrial Myxoma
Left Atrial Myxoma
Rhabdomyoma
Fibroma
Papillary Fibroelastoma
Lipoma
Figure 12.1
Figure 12.2
Figure 12.3
Figure 12.4
Malignant Tumors
Right Atrial Extension of Tumors below the Diaphragm
Chapter 13: Surgery for Atrial Fibrillation
Chapter 13 Introduction
Technique
Omitting Right Atrial Ablation Lines
Figure 13.1
Figure 13.2
Figure 13.3
Figure 13.4
Figure 13.5
Figure 13.6
Figure 13.7
Figure 13.8
Section Iii: Surgery for Congenital Heart Defects
Chapter 14: Patent Ductus Arteriosus
Incision
Surgical Anatomy
Technique for Exposing and Dissecting the Ductus Arteriosus
Technique for Dividing and Ligating the Ductus Arteriosus
Closure of the Ductus Arteriosus in Premature Infants
Completing the Operation
Thoracoscopic Closure of the Ductus Arteriosus
Transcatheter Closure of the Ductus Arteriosus
Calcification of the Ductus Arteriosus
Figure 14.1
Figure 14.2
Figure 14.3
Figure 14.4
Figure 14.5
Figure 14.6
Figure 14.7
Figure 14.8
Figure 14.9
Figure 14.10
Figure 14.11
Anterior Approach to Closure of the Patent Ductus Arteriosus
Technique in Infants and Children
Technique in Adults
Figure 14.12
Figure 14.13
Figure 14.14
Chapter 15: Coarctation of the Aorta
Chapter 15 Introduction
Incision
Surgical Anatomy
Figure 15.1
Exposure of the Coarctation
Figure 15.2
Coarctectomy
Technique with Partial Bypass
Figure 15.3
Fig. 15.4
Figure 15.5
Subclavian Flap Angioplasty
Figure 15.6
Figure 15.7
Figure 15.8
Figure 15.9
Figure 15.10
Long-Segment Coarctation
Figure 15.11
Figure 15.12
Figure 15.13
Reversed Subclavian Angioplasty
Figure 15.14
Extended Resection and Anastomosis
Figure 15.15
Alternate Techniques
Chapter 16: Pulmonary Artery Banding
Chapter 16 Introduction
Incision
Technique
Figure 16.1
Figure 16.2
Adjustable Pulmonary Band Device
Pulmonary Artery Debanding
Figure 16.3
Figure 16.4
Chapter 17: Vascular Ring and Pulmonary Artery Sling
Chapter 17 Introduction
Figure 17.1
Double Aortic Arch
Incision
Technique
Figure 17.2
Figure 17.3
Pulmonary Artery Sling
Incision
Median Sternotomy Technique
Figure 17.4
Figure 17.5
Figure 17.6
Figure 17.7
Chapter 18: Systemic Pulmonary Shunting
Chapter 18 Introduction
Types of Shunts
Modified Blalock–Taussig Shunt with Gore-Tex Tube Graft Interposition
Median Sternotomy Approach
Incision
Technique
Modified Right Blalock–Taussig Shunt
Incision
Technique
Figure 18.1
Figure 18.2
Figure 18.3
Figure 18.4
Figure 18.5
Figure 18.6
Central Shunt
Technique
Figure 18.7
Figure 18.8
Figure 18.9
Prosthetic Ascending Aorta–Right Pulmonary Artery Shunt
Incision
Technique
Figure 18.10
Figure 18.11
Closure of Systemic Pulmonary Shunts
Right-Sided Modified Blalock–Taussig Shunts
Left-Sided Modified Blalock–Taussig Shunts
Central Shunt
Prosthetic Ascending Aorta–Right Pulmonary Artery Shunt
Waterston and Potts Shunts
Technique: Waterston Shunt
Technique: Potts Shunt
Figure 18.12
Figure 18.13
Chapter 19: Atrial Septal Defect
Chapter 19 Introduction
Figure 19.1
Surgical Anatomy of the Right Atrium
Incision
Cannulation
Myocardial Preservation
Figure 19.2
Sinus Venosus Atrial Septal Defect
Technique
Figure 19.3
Figure 19.4
Figure 19.5
Figure 19.6
Ostium Secundum Atrial Septal Defect
Technique
Figure 19.7
Figure 19.8
Figure 19.9
Transcatheter Closure of Atrial Septal Defects
Common Atrium
Figure 19.10
Figure 19.11
Figure 19.12
Right-Sided Partial Anomalous Pulmonary Venous Return
Figure 19.13
Figure 19.14
Left-Sided Partial Anomalous Pulmonary Venous Return
Technique
Figure 19.15
Chapter 20: Total Anomalous Pulmonary Venous Connection
Chapter 20 Introduction
Technique
Intracardiac Type
Infracardiac Type
Supracardiac Type: Superior Approach
Figure 20.1
Figure 20.2
Figure 20.3
Pulmonary Venous Obstruction
Conventional Technique
Sutureless Technique
Figure 20.4
Figure 20.5
Figure 20.6
Figure 20.7
Cor Triatriatum
Surgical Technique
Figure 20.8
Chapter 21: Ventricular Septal Defect
Chapter 21 Introduction
Surgical Anatomy
Figure 21.1
Figure 21.2
Surgical Approach
Cannulation
Myocardial Preservation
Transatrial Approach to a Ventricular Septal Defect
Technique for Closure
Continuous Suture Technique
Figure 21.3
Figure 21.4
Figure 21.5
Figure 21.6
Figure 21.7
Figure 21.8
Figure 21.9
Figure 21.10
Figure 21.11
Transventricular Approach to Ventricular Septal Defect
Interrupted Suture Technique
Figure 21.12
Figure 21.13
Figure 21.14
Figure 21.15
Figure 21.16
Figure 21.17
Subarterial Ventricular Septal Defect
Technique for Closure
Figure 21.18
Muscular Ventricular Septal Defects
Chapter 22: Atrioventricular Septal Defect
Chapter 22 Introduction
Figure 22.1
Figure 22.2
Figure 22.3
Ostium Primum Atrial Septal Defect
Incision
Cannulation
Myocardial Preservation
Technique
Figure 22.4
Figure 22.5
Figure 22.6
Complete Atrioventricular Septal Defect
Cannulation
Two-Patch Technique
One-Patch Technique
One-Patch Technique with Direct Ventricular Defect Closure
Completion of the Operation
Figure 22.7
Figure 22.8
Figure 22.9
Figure 22.10
Figure 22.11
Figure 22.12
Figure 22.13
Unbalanced Atrioventricular Septal Defect
Chapter 23: Right Ventricular Outflow Tract Obstruction
Chapter 23 Introduction
Double-Chambered Right Ventricle
Technique for Repair
Tetralogy of Fallot
Staged Approach
Technique for Complete Repair
Transatrial Technique
Transventricular Technique
Transpulmonary Approach to Pulmonic Valve and Annulus
Figure 23.1
Figure 23.2
Figure 23.3
Figure 23.4
Figure 23.5
Figure 23.6
Figure 23.7
Figure 23.8
Pulmonary Atresia and Ventricula Septal Defect
Technique for Complete Repair
Figure 23.9
Absent Pulmonary Valve Syndrome
Technique
Figure 23.10
Figure 23.11
Figure 23.12
Pulmonary Atresia, Intact Ventricular Septum
Surgical Technique
Definitive Repair
Pulmonary Stenosis and an Intact Ventricular Septum
Technique for Repair
Reoperation on Right Ventricular Outflow Tract
Technique
Figure 23.13
Appendix
Sizing the Pulmonary Outflow Tract
Chapter 24: Left Ventricular Outflow Tract Obstruction
Congenital Aortic Stenosis
Valvotomy Technique
Figure 24.1
Figure 24.2
Resection of the Subvalvular Diaphragm
Figure 24.3
Figure 24.4
Hypertrophic Obstructive Cardiomyopathy
Figure 24.5
Left Ventricular Tunnel Obstruction
Rastan-Konno Aortoventricular Septoplasty
Modified Rastan-Konno Procedure
Figure 24.6
Figure 24.7
Figure 24.8
Figure 24.9
Figure 24.10
Figure 24.11
Figure 24.12
Supravalvular Aortic Stenosis
Figure 24.13
Figure 24.14
Figure 24.15
Figure 24.16
Figure 24.17
Figure 24.18
Figure 24.19
Figure 24.20
Figure 24.21
Figure 24.22
Figure 24.23
Management of Left Ventricular Outflow Tract Obstruction Associated with Other Cardiac Anomalies
Interrupted Aortic Arch with Ventricular Septal Defect
Transposition of the Great Arteries with Ventricular Septal Defect and Left Ventricular Outflow Tract Obstruction
Technique
Figure 24.24
Figure 24.25
Figure 24.26
Figure 24.27
Figure 24.28
Chapter 25: Transposition of the Great Vessels
Chapter 25 Introduction
Surgical Anatomy
Surgical Anatomy of the Right Atrium
Figure 25.1
Figure 25.2
The Arterial Switch Operation
Incision
Preparation
Cannulation
Transection of the Great Arteries
Coronary Artery Reimplantation
Reconstructing the Aorta
Intracardiac Repair
Reconstructing the Pulmonary Artery
Completing the Operation
Figure 25.3
Figure 25.4
Figure 25.5
Figure 25.6
Figure 25.7
Figure 25.8
Figure 25.9
Figure 25.10
Figure 25.11
Figure 25.12
Figure 25.13
Congenitally Corrected Transposition of the Great Arteries
The Senning Procedure
Cannulation
Atrial Incision
The Atrial Septum
The Septal Flap
Sewing the Anterior Edge of the Posterior Segment
Sewing the Posterior Edge of the Anterior Segment
Figure 25.14
Figure 25.15
Figure 25.16
Figure 25.17
Figure 25.18
Figure 25.19
Figure 25.20
Figure 25.21
Figure 25.22
Figure 25.23
The Mustard Procedure
The Baffle
Technique for Preparing the Baffle
Right Atrial Incision
Excision of the Atrial Septum
Baffle Insertion
Figure 25.24
Figure 25.25
Figure 25.26
Figure 25.27
Figure 25.28
Figure 25.29
Figure 25.30
Figure 25.31
Figure 25.32
Figure 25.33
Figure 25.34
Management of Late Complications of the Mustard Procedure
Hemodynamic Deterioration
Baffle Leaks
Obstruction to the Superior Vena Cava
Obstruction to the Inferior Vena Cava
Obstruction to the Pulmonary Veins
Figure 25.35
Figure 25.36
Hemi-Mustard/Rastelli
Figure 25.37
Figure 25.38
Figure 25.39
Chapter 26: Aortopulmonary Window
Chapter 26 Introduction
Figure 26.1
Technique
Figure 26.2
Figure 26.3
Chapter 27: Truncus Arteriosus
Chapter 27 Introduction
Figure 27.1
Incision
Technique
Figure 27.2
Figure 27.3
Figure 27.4
Figure 27.5
Figure 27.6
Figure 27.7
Figure 27.8
Figure 27.9
Truncus Arteriosus with Interrupted Aortic Arch
Chapter 28: Ebstein Anomaly
Chapter 28 Introduction
Figure 28.1
Presentation
Surgery for the Neonate
Technique
Figure 28.2
Surgery beyond Infancy
Technique
Tricuspid Valve Replacement
Figure 28.3
Figure 28.4
Figure 28.5
Figure 28.6
Figure 28.7
Figure 28.8
Figure 28.9
Figure 28.10
Figure 28.11
Figure 28.12
Figure 28.13
Figure 28.14
Chapter 29: Interrupted and Hypoplastic Aortic Arch
Interrupted Aortic Arch
Figure 29.1
Hypoplastic Aortic Arch
Incision
Cannulation
Technique: General
Technique: Interrupted Aortic Arch
Technique: Hypoplastic Aortic Arch
Completion of the Operation
Yasui Procedure
Figure 29.2
Figure 29.3
Figure 29.4
Figure 29.5
Figure 29.6
Figure 29.7
Figure 29.8
Figure 29.9
Figure 29.10
Figure 29.11
Figure 29.12
Chapter 30: The Norwood Principle
Chapter 30 Introduction
Stage I Palliative Reconstruction for Hypoplastic Left Heart Syndrome
Incision
Cannulation
Procedure
Figure 30.1
Figure 30.2
Figure 30.3
Aortic Arch Reconstruction
Patch Reconstruction Technique
Direct Anastomotic Arch Reconstruction
Figure 30.4
Figure 30.5
Figure 30.6
Figure 30.7
Figure 30.8
Figure 30.9
Figure 30.10
Figure 30.11
Figure 30.12
Pulmonary Blood Flow
Right Ventricle-Pulmonary Artery Shunt
Systemic–Pulmonary Shunt
Figure 30.13
Figure 30.14
Figure 30.15
Figure 30.16
Figure 30.17
Damus–Kaye–Stansel Procedure
Incision
Cannulation
Procedure
Completion of the Operation
Figure 30.18
Figure 30.19
Figure 30.20
Chapter 31: The Fontan Principle
Chapter 31 Introduction
Pathophysiology of a Single Ventricle
Surgical Management
Management after the Neonatal Period
Bidirectional Glenn Procedure
Cannulation
Completing the Shunt
Figure 31.1
Figure 31.2
Bidirectional Glenn on Cardiopulmonary Bypass
Hemi-Fontan Procedure
Technique
Figure 31.3
Figure 31.4
Figure 31.5
Figure 31.6
Completion Fontan Procedure
Total Cavopulmonary Connection
Incision
Cannulation
Technique for the Extracardiac Fontan Procedure
Technique for a Lateral Tunnel Fontan Procedure
Completing the Operation
High-Risk Candidates for the Fontan Procedure
Technique
Figure 31.7
Figure 31.8
Figure 31.9
Figure 31.10
Figure 31.11
Figure 31.12
Figure 31.13
Chapter 32: Coronary Artery Anomalies
Chapter 32 Introduction
Anomalous Left Coronary Artery from the Pulmonary Artery
Surgical Anatomy
Incision
Technique
Figure 32.1
Figure 32.2
Figure 32.3
Figure 32.4
Coronary Fistulae
Technique
Anomalous Coronary Artery Origin and Course between Great Vessels
Technique
Figure 32.5
| An aparitie | 05 Oct 2016 |
| Autor | Abbas Ardehali , Jonathan M. Chen |
| Dimensiuni | 21.84 x 2.03 x 27.94 cm |
| Editura | LWW |
| Format | Hardcover |
| ISBN | 9781451183689 |
| Limba | Engleza |
| Nr pag | 448 |
| Versiune digitala | DA |
-
84000 lei 81000 lei
Clientii ebookshop.ro nu au adaugat inca opinii pentru acest produs. Fii primul care adauga o parere, folosind formularul de mai jos.